Oncology Case 6
Oncology Case 6
a) Immediate biopsy
b) Repeated 18F-FDG PET/CT in 3 months
c) No further evaluation needed due to negative bone scan and 18F-FDG PET/CT
d) Further evaluation (e.g., MRI, follow-up imaging, or biopsy)
Scroll down for answer
Answer: d
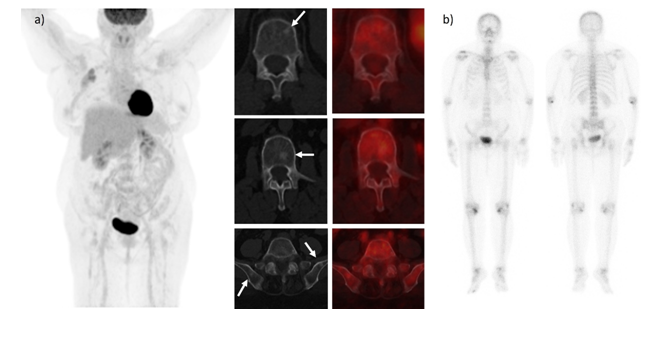
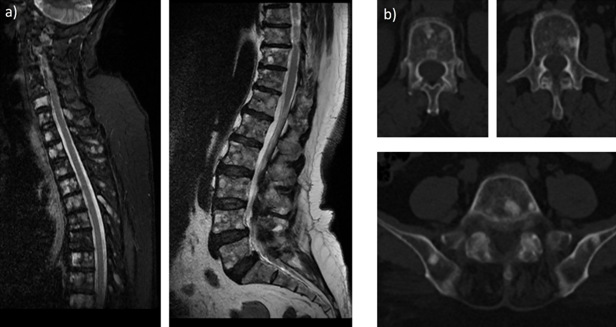
a) MRI shows evidence of extensive abnormal marrow signals involving almost the whole spine vertebral bodies, bilateral sacral ala and iliac bones, suggestive of disseminated bone metastasis.
b) Follow-up CT scan shows interval increase in sclerosis at multiple sclerotic bone lesions suggesting healing response.
Invasive lobular carcinoma (ILC) is the second most common breast carcinoma, accounting for 10% to 15% of invasive breast carcinomas. 18F-FDG PET/CT plays a vital role in the management of breast cancer patients for staging and restaging setting based on the principle of increased glucose utilization by tumor cells. However, the sensitivity of 18F-FDG PET/CT is lower in lobular carcinoma and low-grade breast tumors [1 ]. The ILC may demonstrate low detection rates on 18F-FDG PET due to lower FDG-avidity in tumor cells [2 ]. Invasive lobular carcinomas demonstrate lower SUV max than invasive ductal carcinoma(IDC) due to lower tumor cell density, decreased proliferation rate, diffuse infiltration of surrounding tissue and low level of GLUT-1 expression, in ILCs [ 3].
Osseous metastases are more commonly sclerotic in patients with ILC as compared to IDC, however the reason behind this is unclear. A possible hypothesis could be due to greater bone remodeling in ILC osseous metastases, owing to its slower tumor growth or less dense packing of tumor cells. 18F-FDG PET/CT PET is more sensitive in detecting lytic osseous metastases in patients with breast cancer, while MDP bone scan is more sensitive in the detection of sclerotic osseous metastases. However, diagnosis of bone metastases in the ILC is always challenging and a lot of false negative cases are seen with both bone scan and 18F-FDG PET/CT scan. MRI is more accurate in diagnosing bone metastasis in lobular breast cancer. It detects bone metastases at an earlier stage than other imaging techniques. It can identify subtle changes in bone marrow that may not be visible on bone scan, 18F-FDG PET or CT scans. The misdiagnosis rate of MRI is relatively low in the diagnosis bone metastasis in lobular breast cancer [4 ]. Non-FDG-avid sclerotic osseous metastases were significantly more common in untreated patients with ILC than with IDC. The diagnostic confidence is lower in 18F-FDG PET/CT in ILC when evaluating for osseous metastases and consideration given to performing a biopsy/MRI or obtaining follow-up imaging before excluding metastatic disease
A recent study by Usmani et al [5] indicate that 18F-FDG PET/CT demonstrated low sensitivity (33.33%) and accuracy (76.19%) in detecting bone metastases in lobular breast cancer patients. Sclerotic bone metastases in lobular breast cancer often show lower 18F-FDG avidity, leading to false negatives. The study highlights the need for careful evaluation of any sclerotic lesion in lobular breast cancer patients, even if negative on 18F-FDG PET/CT and suggest that alternative imaging modalities or more specific PET tracers such as 18F-fluoroestradiol (FES),
68Ga-FAPI-04, and 89Zr-Trastuzumabmay be necessary for comprehensive evaluation of lobular breast cancer metastases.
- Hogan MP, Goldman DA, Dashevsky B, et al. Comparison of 18F-FDG PET/CT for systemic staging of newly diagnosed invasive lobular carcinoma versus invasive ductal carcinoma. J Nucl Med. 2015;56:1674–1680.
- Jung NY, Kim SH, Kim SH, et al. Effectiveness of breast MRI and (18)F-FDG PET/CT for the preoperative staging of invasive lobular carcinoma versus ductal carcinoma. J Breast Cancer. 2015;18:63–72
- Bos R, van Der Hoeven JJ, van Der Wall E, van Der Groep P, van Diest PJ, Comans EF, et al. Biologic correlates of (18)fluorodeoxyglucose uptake in human breast cancer measured by positron emission tomography. J Clin Oncol. 2002;20:379–87.
- Rong Y, Ren H, Ding X. MRI and Bone Scintigraphy for Breast Cancer Bone Metastase: A Meta-analysis. Open Med (Wars). 2019;14:317-323.
- Usmani S, Al Riyami K, Jain A, Alajmi AA, AlBaimani K, Dumasig P, Al Busaidi A, Al Sukati R. Enhancing precision in bone metastasis diagnosis for lobular breast cancer: reassessing the role of 18F-FDG PET/CT. Nucl Med Commun. 2024